Medicare telehealth coverage will remain available for patients receiving care from home under a temporary federal extension, preserving pandemic-era access rules that were set to expire. The measure maintains broad eligibility for virtual visits but stops short of permanent reform, leaving patients, providers, and insurers facing renewed uncertainty about the future of remote care in the United States.
Table of Contents
Medicare Coverage
| Key Issue | Current Status |
|---|---|
| Home-based telehealth | Covered temporarily |
| Geographic limits | Waived under extension |
| Audio-only visits | Allowed for select services |
| Expiration date | Early 2026 |
How Medicare Telehealth Coverage Reached This Point
Pre-Pandemic Restrictions
Before 2020, Medicare telehealth coverage was narrowly defined. Patients typically had to live in rural areas and travel to an approved medical facility to qualify. Care delivered to a patient’s home was generally excluded, reflecting concerns about cost control and program oversight.
These restrictions limited adoption, even as telehealth technology advanced and commercial insurers expanded virtual care offerings.
Rapid Expansion During COVID-19
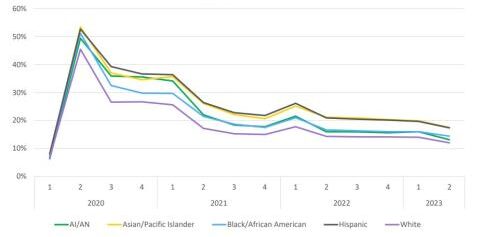
The COVID-19 pandemic forced a rapid policy shift. Congress and federal health agencies waived geographic and originating-site requirements, allowing beneficiaries nationwide to receive telehealth services from home.
Utilization surged. According to data from the Centers for Medicare & Medicaid Services (CMS), telehealth visits among Medicare beneficiaries increased by more than forty-fold in the first year of the pandemic, transforming how care was delivered.
Health systems invested heavily in digital infrastructure, and many patients — particularly older adults managing chronic conditions — reported improved access and convenience.
What the Current Extension Preserves
Core Elements of Medicare Telehealth Coverage
Under the current policy extension, Medicare telehealth coverage continues to allow:
• Virtual visits from a patient’s home
• Removal of rural-only eligibility requirements
• Expanded provider participation
• Coverage for certain audio-only services
CMS officials say the goal is continuity. “Abrupt policy reversals create confusion for beneficiaries and providers alike,” a CMS spokesperson said in recent guidance.
The Cost Question: Savings or Spending Risk?
Supporters Cite Efficiency Gains
Advocates argue that Medicare telehealth coverage reduces costs by preventing hospitalizations, improving chronic disease management, and lowering transportation barriers.
A 2023 analysis from the Department of Health and Human Services found telehealth reduced missed appointments and improved follow-up care for patients with diabetes, heart disease, and mental health conditions.
Critics Warn of Overuse
Skeptics raise concerns about increased utilization rather than substitution. Some lawmakers worry telehealth may add visits rather than replace in-person care, driving up overall spending.
The Medicare Payment Advisory Commission (MedPAC) has urged caution, recommending stronger data collection before making permanent coverage decisions.
Fraud, Oversight, and Program Integrity
A Growing Enforcement Focus
Federal investigators have flagged telehealth fraud as a growing concern. Several high-profile cases involved billing for unnecessary durable medical equipment or services never delivered.
The Department of Justice has increased enforcement actions tied to telehealth billing, emphasizing that flexibility does not mean reduced oversight.
CMS has responded by tightening documentation requirements and expanding audit authority, even as coverage remains in place.
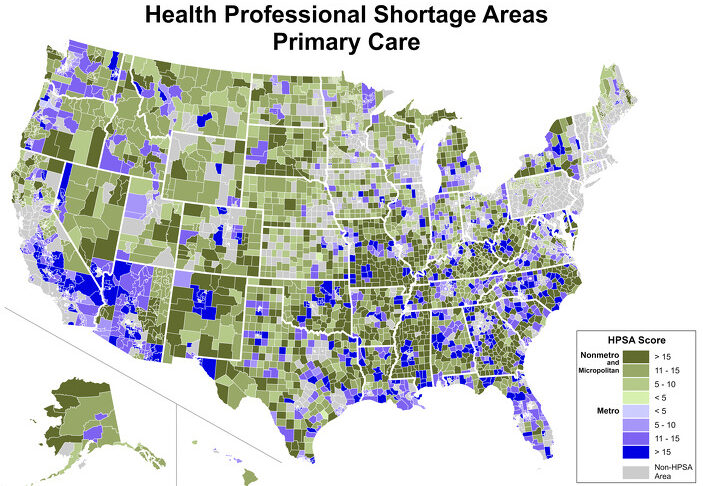
Rural and Homebound Patients: Who Benefits Most?
Access Beyond Geography
For rural beneficiaries, telehealth reduces travel times that can exceed several hours. For urban patients, especially those with mobility limitations, home-based care eliminates transportation and caregiver burdens.
According to the Kaiser Family Foundation, nearly one in four Medicare beneficiaries lives with a disability that makes travel difficult, underscoring the stakes of potential rollbacks.
Medicare Advantage vs. Traditional Medicare
Diverging Coverage Paths
While Original Medicare relies on congressional action, Medicare Advantage plans often have broader flexibility. Many plans have already incorporated telehealth as a standard benefit, regardless of federal waivers.
Industry analysts note this could widen disparities between beneficiaries depending on plan enrollment, particularly if traditional Medicare rules revert.
A Patient’s Experience
For 72-year-old Margaret Lewis of Ohio, telehealth transformed her care. Managing arthritis and hypertension, she relies on monthly virtual check-ins with her primary care physician.
“Without telehealth, I would need help getting to appointments every few weeks,” Lewis said. “It has kept me independent.”
Patient advocacy groups argue stories like hers should weigh heavily in future policy decisions.
Political and Legislative Outlook
Bipartisan Interest, No Consensus
Telehealth enjoys broad public support, but permanent legislation has stalled amid debates over cost, fraud prevention, and quality standards.
Several bipartisan bills propose phased permanence tied to outcome data, while others call for targeted coverage limited to behavioral health and chronic care management.
Congressional aides say negotiations are likely to continue into 2026.
How the U.S. Compares Globally
Other countries have taken different approaches. The United Kingdom’s National Health Service expanded telehealth during the pandemic but later emphasized hybrid care models. Canada has moved toward provincial permanence, particularly for rural care.
Health policy experts say the U.S. debate reflects its fragmented payer system rather than a lack of evidence.
What Patients Should Do Now
• Confirm telehealth eligibility with providers
• Monitor Medicare notices for policy updates
• Ask Medicare Advantage plans about long-term coverage
• Stay alert to legislative developments
CMS encourages beneficiaries to use official Medicare resources rather than third-party advertisements to avoid scams.
Final Context
For now, Medicare telehealth coverage remains intact, preserving access that millions of beneficiaries have come to rely on. Whether that access becomes permanent will depend on political compromise, cost evidence, and how policymakers balance flexibility with oversight.
As one congressional health staffer put it, “Telehealth is no longer an experiment. The question is how we regulate it, not whether it exists.”
FAQ
Is telehealth from home still covered by Medicare?
Yes, under the current extension, eligible services remain covered.
Will telehealth coverage end?
Coverage may change if Congress does not pass permanent legislation.
Are phone-only visits covered?
Some audio-only services remain eligible under specific rules.
Does Medicare Advantage offer more telehealth?
Often yes, depending on the plan.